Care from a Hospital Setting
structures that facilitate integrated discharge and follow-up planning
Keywords: hospital discharge, palliative care, multidisciplinary working, end of life care
Protected hospital discharge and palliative care teams
Summary
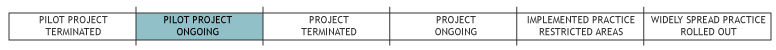
This pilot project takes place in the Region of Umbria in central Italy and is run by a Local Health Authority (LHA 2 Umbria). The project involves different organisations and service providers such as hospitals, hospices and regional home care services. These organisations have set up a small multi-professional team to facilitate ‘protected’, i.e. integrated discharge processes for terminally ill patients. The strategic objective of the project is to improve quality of health services and assistance for patients by creating integrated care pathways among hospitals, local health services (home care) and residential assistance (hospice).
What is the main benefit for people in need of care and/or carers?
The example meets the widespread need of terminally ill patients and their families to find support during crises, to assure health and social assistance, and to facilitate a smooth transition from hospital to home care.
What is the main message for practice and/or policy in relation to this sub-theme?
The implementation of this service showed most promising results:
- lower rates of calls to emergency service and hospitalization in the last 48 hours of life (unsuitable inappropriate hospitalization)
- shorter length of stay in hospital (with subsequent lower costs for the health system)
- increased use of opiate drugs (usually noted as a common indicator for quality palliative care)
- assistance for families in managing illness and bereavement.
These indicators show the highly preventive character of an integrated system for terminally ill patients.
Why was this example implemented?
At the origins of this project was a significant tendency towards the hospitalisation of patients in need of palliative care in the Local Health Authority 2 of the Italian Region Umbria (LHA 2 Umbria). For instance, still in 2006, 86 of 950 oncological patients of Perugia’s Hospital died within the hospital where staff was not adequately prepared and premises were not appropriate to care for terminally ill patients.
Therefore, the regional government and the LHA 2 decided to implement a new organisational model with the aim to reduce health and social care expenses by providing better services and improved quality of life for terminally ill patients. The regional government wanted to particularly support local palliative care services to simplify discharge from hospital with a view to offering suitable services and continuing care.
First directions about palliative care were given with the Regional Health Plan 1999-2001 that was underpinned by a “Regional Project to create a network for assisting terminally ill patients” (Law 39/1999). However, it was only in 2004 that directions for Local Health Authorities about the organisation of palliative care and pain therapy services were legally defined in Umbria.
In the meantime, two additional research projects (2006-2007 and 2010) were carried out in the area to create and share an organisational model to improve integration of home care services and to promote the implementation of pathways for continuing care of terminally ill patients.
Description
Today, assistance for terminally ill patients in Umbria is provided through a network of community care services and structures that replace hospital care. In the Local Health Authority 2 (LHA), the network is composed of GPs, Health Centres supplying home care, a small palliative care team and a hospice providing residential places. Two voluntary organisations complete the network, offering assistance and support to patients and their families, e.g. emotional support, counselling, hands-on care.
The project aims at integrating palliative care into home care and hospital services:
- to avoid inappropriate hospitalisation at the end of life;
- to assure palliative care and assistance at home or in a hospice;
- to reduce aggressive therapeutic treatments;
- to promote pain controlling treatments and treatment for other symptoms; and
- to address psychological and social problems of patients and their families.
The small palliative care team usually meets once a week in the hospital to assess the patient’s conditions and to plan for care at home or in the hospice. The team consists of a palliative care doctor, the hospice’s head nurse, a hospital doctor, the hospital’s head nurse and, if necessary, the hospice’s social worker and psychologist. Hospice staff thus meet patients and their families directly in the hospital upon request of hospital staff, patients and/or families. Families who agree with a transfer may visit the hospice and are informed about its organisation. The team meetings and the opportunity to meet patients and families in the hospital facilitate a coordinated discharge and the continuity of care.
The team is involved in the delivery of palliative care both in the hospice and at home. From January 2010 to June 2010, 358 patients have been discharged from hospital with a coordinated pathway accompanied by the palliative care team.
Palliative care is provided free of charge for patients as expenses are covered by the regional health system both for hospital and for home care services. In fact, facilitating ‘protected’ discharge processes is cheaper than keeping a patient in the hospital: the mean cost per day in a hospital is about €800 per day (mean cost for oncologic patients from a research by Umbria Region in 2010 – see references) and, as the mean length of stay is about 11 days (mean length of stay in hospital for oncologic patients from the same research), the average cost for each individual patient is about €8,800. As the mean costs for integrated home care after discharge amount to about €60 per day (mean cost for an intensive level of home care from the same research) and since the terminal phase on average lasts about 30 days, the total cost for a palliative care patient at home is about €2,000. Even if this sum does not include the costs for GPs and the palliative care team, i.e. professionals working for and remunerated by the National Health System anyway, it indicates the financial advantages of palliative care outside the hospital.
What are/were the effects?
Creating integrated care pathways among hospitals, local health services and residential assistance is a strategic objective to improve quality of care for patients and families (reducing feelings of abandonment) and for health services (access and suitability of care, chronic care management, suitable placement).
Research (Regione Umbria, 2010) funded by the Umbria Region clearly showed that in the Districts where no support network had been installed, the following inconveniences persisted:
- There were higher rates of emergency calls and a higher share of hospitalisation during the last 48 hours of life (inappropriate hospitalisation)
- Length of stay in hospitals was longer – with subsequent higher costs for the health system
- Less opiate drugs were used which is usually known as an indicator for a worse quality of (palliative) care
- Families lacked support in managing illness and loss.
The same research (Regione Umbria, 2010) found that, in districts where palliative care teams and coordinated discharge pathways have been installed, terminally ill patients have a better quality of life and more support: less inappropriate hospitalisation, less likelihood to die in a hospital, and a higher use of opiate drugs.
What are the strengths and limitations?
Strengths
- The project supported cooperation among competent services in order to plan coordinated discharge, care and assistance (hospital-hospice-home service). This collaboration improved terminally ill patients’ life and reduced number of inappropriate hospitalization ad lowered in-hospital deaths.
- Active support of voluntary associations (in LHA 2 Umbria area works two associations that offer, for example, emotional support, counselling, hands on care). The project encouraged integration between the associations’ activities in home care system.
- Specific research for implementing and supporting integrating system (see rationale). Umbria Region financed and promoted special research and projects to support system development.
Weaknesses
- Lack of a Unique Access Point for home care in every district. The project promoted a wider integration among services, but even today specialised palliative care services may be activated directly without the involvement of Districts’ Health Centres.
Opportunities
- It reduces expenses in charge of SSN with equal services (i.e. reduction of stay in hospital).
- It reduces emergency calls and hospitalisation in the last 48 hours of life (unsuitable hospitalisation).
- It spreads a palliative care ‘culture’ and helps improve pain management by means of opiate drugs.
- It promotes assistance to families in order to manage illness and bereavement.
Threats
- Organisational procedures are based on habits rather than on formalised practices, despite existing operational protocols.
- Communication difficulties persist among different professionals (hospital doctors, GPs, palliative care doctors, nurses, physiotherapists, voluntary operators, etc.) and among different services taking care of terminally ill patients.
Credits
Author: Patrizia Di SantoReviewer 1: Laura Holdsworth
Reviewer 2: Pierre Gobet
Verified by: Georg Ruppe
External Links and References
Peer reviewed journals/systematic reviews:
- Bietta C, Vallesi G, Petrella M (2009) ‘Hospital admission in terminally ill cancer patients: a survey in the Umbrian Local Health Unit 2’ in: Epidemiol Prev., Vol. 33(6): 233-8 (Italian).
Policy documents:
- Progetto aziendale di cure palliative nella AUSL n. 2
- AUSL 2 Regione Umbria, Sistema delle cure domiciliari, Decisione amministrativa n. 684/2004 (delibera cure domiciliari e allegato)
- AUSL 2 Regione Umbria, Cure domiciliari, target, attivazione e presa in carico, livelli di complessità assistenziale e tipologia delle prestazioni erogate (allegato alla delibera)
National and EU funded project reports:
- Regione Umbria. Ricerca scientifica finalizzata alla programmazione socio-sanitaria regionale. Bando pubblico, competenza 2008, DGR 20 ottobre 2008 n.1405, Dimissioni protette di pazienti terminali che necessitano cure palliative attraverso la costruzione della rete tra ospedale, servizi territoriali e hospice
- Regione Umbria. Ricerca scientifica finalizzata alla programmazione socio-sanitaria regionale. Bando pubblico, competenza 2003, DGRU 1375/24 settembre 2003. Progetto: “Integrazione delle cure palliative nel sistema delle cure domiciliari. Modelli di implementazione e valutazione di percorsi assistenziali integrati nell’assistenza ai pazienti affetti da malattie evolutive irreversibili che necessitano di cure palliative”
Unpublished/web-based documents (policy documents, practice reports)
- Regione Umbria, Ausl 2 Umbria, Dimissioni protette di pazienti terminali che necessitano cure palliative attraverso la costruzione della rete tra ospedale, servizi territoriali e hospice, Report, 2010
- Regione Umbria, Ausl 2 Umbria, Cure Palliative, Funzionamento organizzativo e percorsi di assistenza, Report, 2007
- AUSL 2 Regione Umbria, Modello e procedure d’integrazione delle cure palliative nel sistema delle cure domiciliari, Bozza di documento (versioni novembre e dicembre 2004)
- Regione Umbria, L’organizzazione del servizio ADI “Cure palliative” nel Distretto Socio-sanitario dei Base n. 4 di Spoleto

